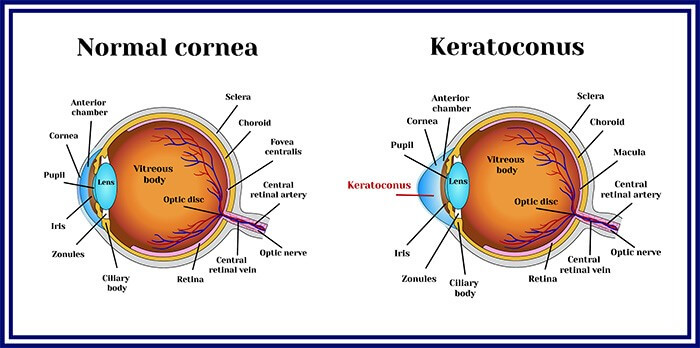
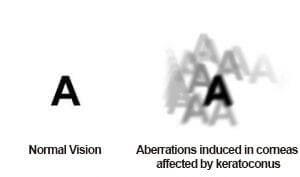
Keratoconus (kerato : cornea, conus : cone like) is a non-inflammatory thinning and anterior protrusion (ectasia) of the cornea (the central portion of the cornea begins to thin and bulge out like a cone) that results in steepening and distortion of the cornea, altered refractive error, myopia, irregular astigmatism halos, monocular double-vision, ghost images and sensitivity to light and decreased vision. . When light enters the eye, it first passes through the cornea. If the cornea has turned conical or irregular, there is distortion of the image. The eye develops astigmatism (cylindrical errors) and myopia [shortsightedness] and the vision may become severely blurred
Keratoconus is a common progressive, bilateral (but usually asymmetric, one eye being more involved than the other) corneal condition, occurring in about 20 in 1000 people in India. The condition typically starts in adolescence and early adulthood. Usually one eye is involved more than the other. It is more common in people with allergies or those who rub their eyes frequently.
The cornea is the clear regular spherical dome shaped window on the front of the eye. Normal pressure within the eye causes the cornea to bulge forward into an irregular cone shape in keratoconus. The substance of the cornea consists of hundreds of layers that are linked to each other by a substance called collagen. If these collagen cross-links between stromal layers are lost as in keratoconus, there is a progressive corneal thinning and stretching which gradually progresses, and leads to corneal surface distortion and corneal scarring in advanced cases and occurs often in both eyes
Early diagnosis and treatment of keratoconus is important, more so in children and adolescents. About 13% of keratoconus patients have other family members with the disease. LASIK or SMILE should not be done in Keratoconus as it can weaken the cornea even more and make your vision worse.
Despite its uncertainties, keratoconus can be successfully managed with a variety of clinical and surgical techniques, and often with little or no impairment to the patient's quality of life. Grover Eye Laser & ENT Hospital is one of the pioneer institutions in management of keratoconus.
Keratoconus is a complex condition of multifactorial etiology. Both genetic and environmental factors are associated with it. Reported risk factors for keratoconus include eye rubbing, a family history of keratoconus, ocular allergy, connective tissue disease, during pregnancy in some and long-term contact lens wear. It affects men and women in equal proportions and affects both eyes sooner or later in 90% of patients.
At early stages, the symptoms of keratoconus may be no different from just having the need for spectacle correction. These symptoms usually first appear in the late teens and early twenties. As the disease progresses, the vision deteriorates further and along with blurring there is distortion of vision and increased sensitivity to light and glare. They may require frequent change of glasses and later perfect vision is not possible with any glasses.

In the advanced stage, the patient may experience a sudden clouding of vision in one eye that clears over a period of weeks or months. This is called “Acute hydrops” and is due to the sudden entry of fluid into the stretched cornea. In advanced cases, superficial scars form at the apex of the corneal bulge resulting in more vision impairment.
A complete assessment for keratoconus includes
1.Refraction and visual acuity evaluation
2.Intraocular pressure measurement
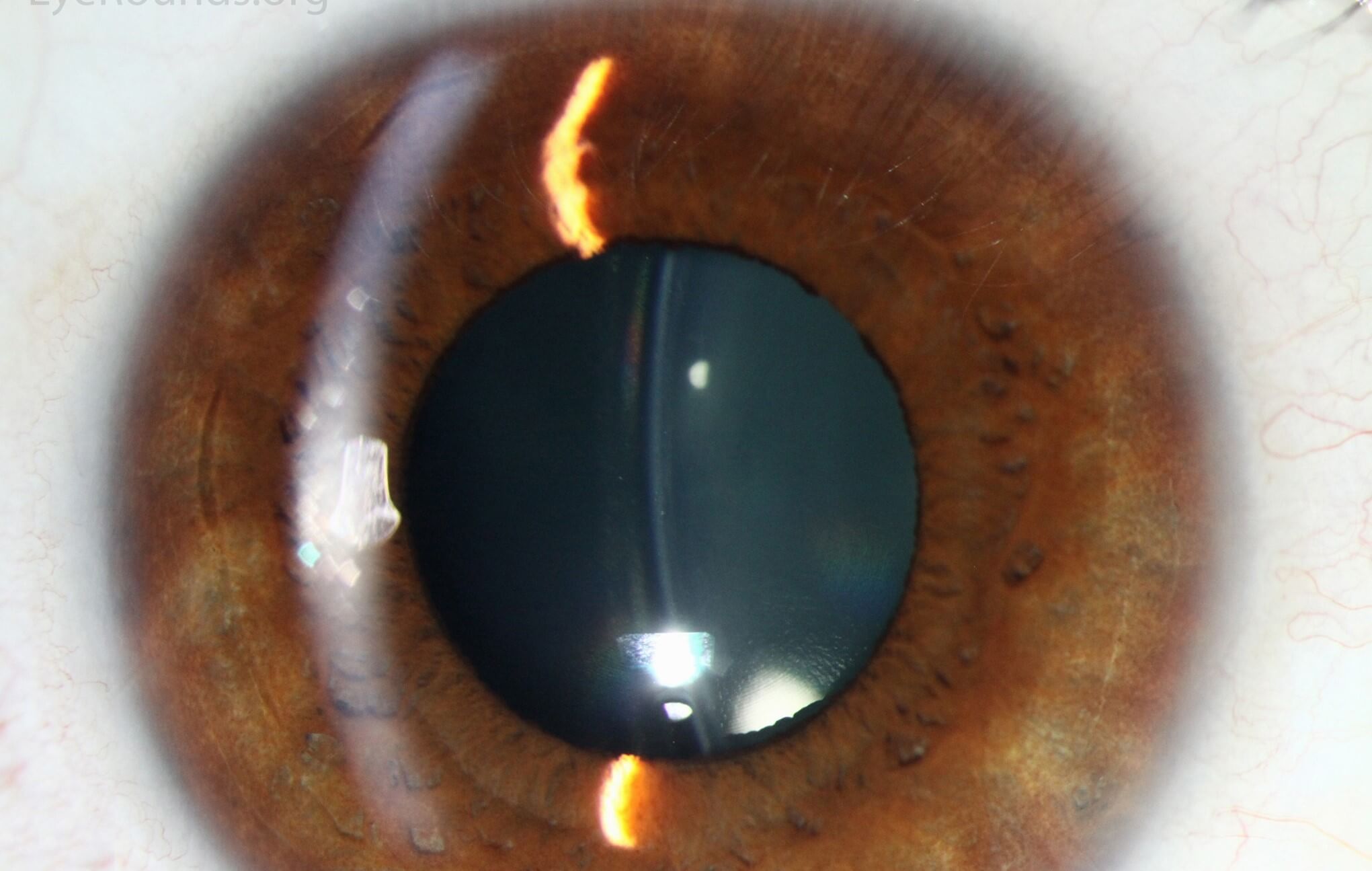
3.Slit lamp examination and retina evaluation is done by an ophthalmologist with a detailed eye examination. Diagnosing mild or early disease may be difficult as it does not show any identifiable signs on slit-lamp examination.
4. OPD Scan, Corneal Topography / Pentacam
Advanced topography systems such as the Pentacam and Orbscan assess the overall architecture of the cornea and help in early detection of keratoconus.
CORNEAL TOPOGRAPHY TEST
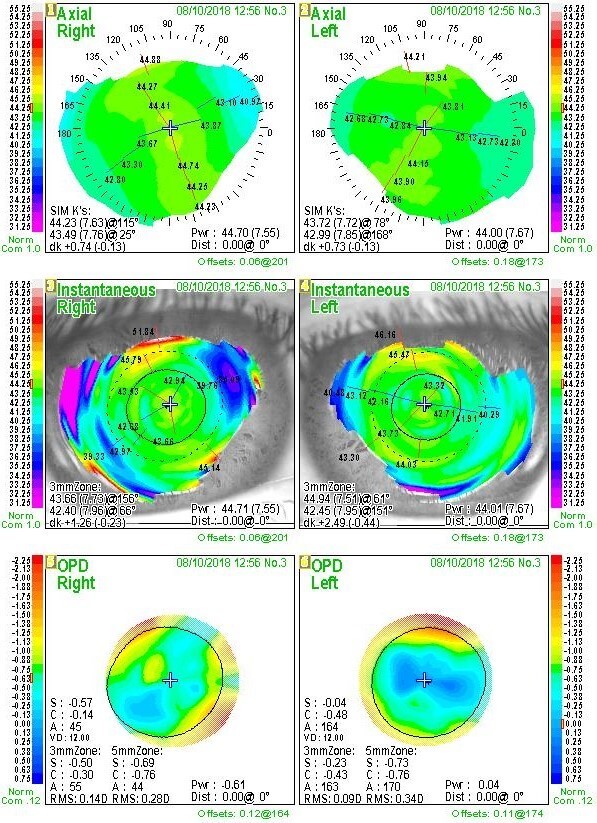
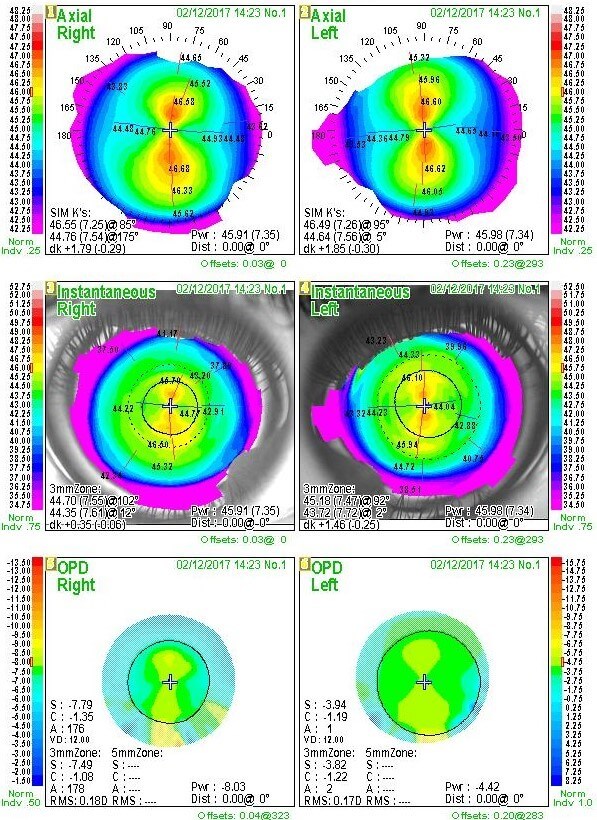
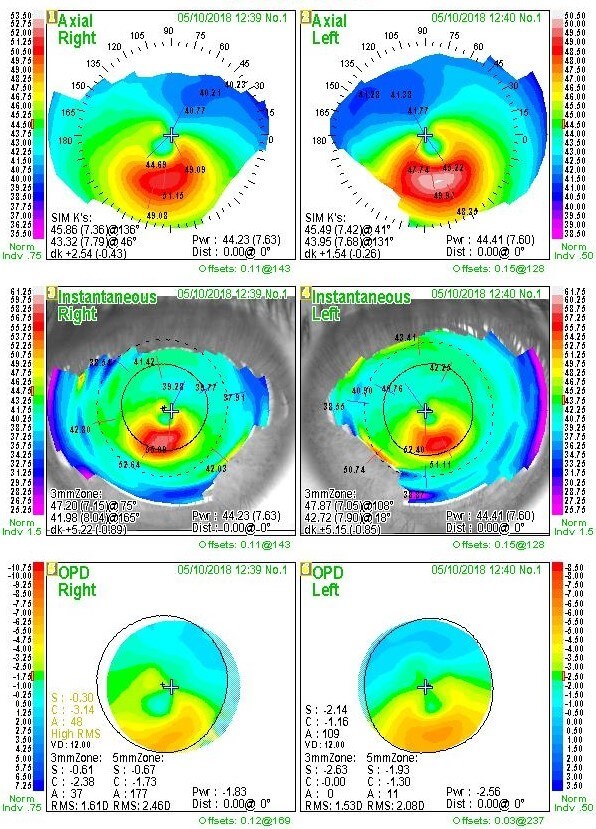
SPHERICAL REGULAR ASTIGMATISM KERATOCONUS
The topographical map reveals distortions or scarring in the cornea, with keratoconus revealed by a characteristic steepness of curvature which is usually below or around the centre of the cornea. The topography is used for assessing its rate of progression and in deciding the appropriate treatment options. A more definitive diagnosis can be obtained using the advanced scan corneal topography, in which an automated instrument projects an illuminated pattern onto the cornea and determines its shape from analysis of a digital image.
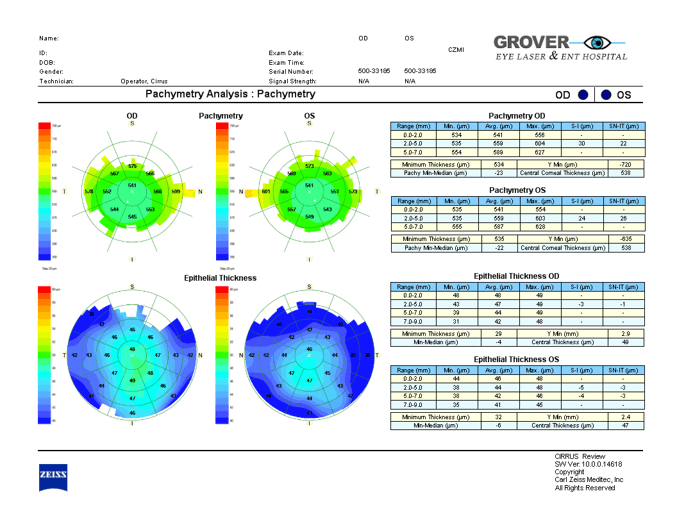
5.Corneal Thickness measurement, Pachymetry : Measures corneal thickness in microns for multiple locations of the cornea. It may be measured with an ultrasonic probe or by pentacam / AS-OCT.


There are two aspects to keratoconus treatment
First we need to stop progression for which the most widely accepted treatment is C3R or corneal crosslinking. Alternatives are Keraflex, KXL.
Second step is to correct or at least improve the errors of vision (refractive errors). These options include: Spectacles, RGP contact lenses, special keratoconus contact lenses, INTACS (intracorneal ring segments) and ICL, topography-guided PRK (TG-PRK) or advanced TG-ASA (or a combination of various options. The decision as to what is best suited for your eyes can only be taken after a complete assessment. Advanced cases with extreme thinning or scarring may not be amenable to treatment with these modalities. A lamellar or full-thickness corneal transplant is required in such cases.
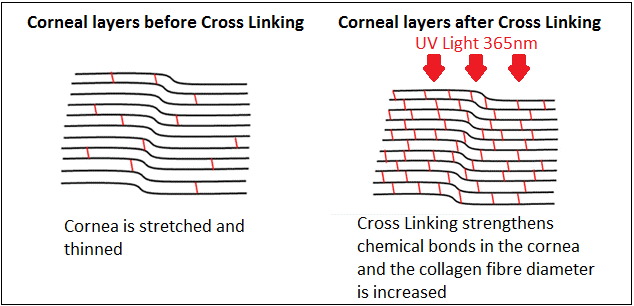
Corneal Collagen Crosslinking with Riboflavin (abbreviated to C3R) LINK also called Crosslinking CXL is the globally accepted first line treatment for stabilization of the corneal ectasia (bulge) in keratoconus. C3R causes the collagen fibrils to thicken, stiffen, and crosslink & re-attach to each other, making the cornea stronger and more stable thus convincingly halting the progression of the disease.
This treatment is aimed at arresting the further progression of keratoconus by strengthening the corneal architecture (biomechanical strength). Biomechanical measurements have shown an impressive increase in corneal rigidity of over 300% after crosslinking. and thereby prevent further deterioration in vision and frequently averts the need for corneal transplantation later.
Glasses or contact lenses (or some other treatment) will still be needed following the cross-linking treatment, although a change in the prescription may be required.
We have over 10 years’ experience with C3R, and now with accelerated CXL.
Like all treatments, this procedure is most beneficial when performed at the earliest possible stage of Keratoconus when the visual and mechanical damage to the cornea is minimal.
Results have been very promising with the slowing or cessation of keratoconus progression in almost 100% of eyes.
Accelerated Crosslinking involves use of latest equipment in crosslinking which delivers same energy in shorter period of time ( 3 to 9 minutes) making the total procedure to be over in less than half an hour. This treatment offers less patient discomfort and early recovery and is most popular in our hospital now.
In the conventional C3R protocol, a minimum de-epithelialized corneal thickness of 400 μm is recommended to avoid potential irradiation damage to the corneal endothelium cells. In advanced keratoconus, however, stromal thickness is often lower than 400 μm, which limits the application of C3R in that category.
Trans-epithelial CXL, customized epithelial removal, contact lens or Smile lenticule assisted CXL, Iontophoresis-assisted transepithelial CXL are the variations available for such patients.
Safe CXL in thinner corneas can also be achieved by making alterations in riboflavin concentration, UV exposure time and UV light intensity. Such protocols are being regularly followed by the doctors in our hospital.


PROCEDURE Of collagen collagen cross-linking (C3R)
A treatment modality for keratoconus which has shown great success is Corneal Collagen Crosslinking with Riboflavin (C3-R®*). This method works by increasing collagen cross-linking, which are the natural “anchors” within the cornea. These anchors are responsible for preventing the cornea from bulging out and becoming steep and irregular (which is the cause of keratoconus).
The riboflavin, when activated by approximately 30 minutes illumination with UV-A light (365 - 370nm), augments the collagen cross-links within the stroma and so recovers some of the cornea's bio-mechanical strength and in some cases even reverse it. This process creates new chemical bonds (cross-links) between collagen fibrils and other extracellular matrix proteins in the corneal stroma through localized photo polymerization.
The treatment is performed in our operation theatre under complete sterile conditions. The treatment is performed under topical anesthesia (using anesthetic eye drops). The surface of the eye (cornea) is treated with application of Riboflavin eye drops for 30 minutes. The eye is then exposed to UVA light for 30 minutes. Hence, the treatment takes about an hour per eye. After the treatment, antibiotic eye drops are applied; a bandage contact lens may be applied, which will be removed by our doctor during the follow up visit.
C3R CSO Vega - Keratoconus Treatment
After the procedure a bandage contact lens is applied. You may experience pain, lid swelling and foreign body sensation for 2 to 3 days after the procedure. The contact lens is removed 3 to 4 days after the epithelial healing is complete.
Treatment of mild keratoconus is geared towards eliminating or reducing the myopia and astigmatism, at times with spectacles alone.
As the condition progresses, spectacles may no longer provide the patient with a satisfactory degree of visual acuity, and most doctors will move to managing the condition with rigid contact lenses . Initial management is tried with rigid contact lenses by our hospital contact lens specialist.
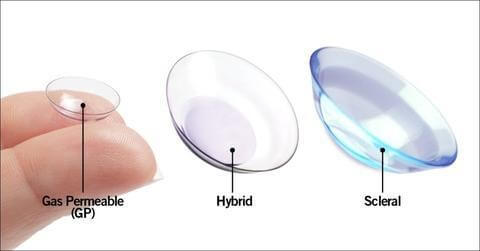

There is a small risk of infection with use of contact lens so it is important to strictly follow the hygiene instructions given at the hospital when the contact lenses are fitted.
Contact lenses are used as temporary measures of treatment, but do not, unfortunately, slow down the rate of progression of the cone. These are quite useful after stabilization of keratoconus with C3R.
In about 10% to 20% of keratoconus patients the cornea may become extremely steep, thin and irregular or the vision cannot be improved sufficiently with contact lenses. The cornea may then need to be replaced surgically with a full-thickness corneal graft (PKP) or lamellar corneal transplant or grafting (keratoplasty), DLK etc. Visual recovery after a transplant takes a long time - sometimes as long as a year to 18 months - to settle down and there is a strong possibility that the eye will still need to be fitted with a contact lens or some other procedure afterwards also in order to see properly.
There is also a risk of the transplant rejecting afterwards, although a majority of corneal transplants done for keratoconus are successful.
To get better vision after corneal grafting contact lenses or additional corneal laser vision correction, TG-ASA may be needed.
Intacs / Corneal ring segment insert link is a type of implant, another surgical alternative to corneal transplant / number correction in keratoconus. It involves insertion of thin plastic PMMA, semi-circular intrastromal corneal ring segments to provide more structural stability. The placement of Intacs remodels and reinforces the cornea, eliminating some or all of the irregularities caused by keratoconus in order to provide improved vision.
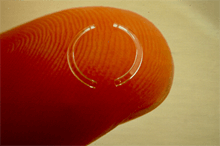

Intacs link are thin plastic PMMA, semi-circular rings inserted into the middle layer of the cornea. The channels for placement of INTACs into the cornea can be created mechanically with a special instrument or with a precise femtosecond laser.
A small incision is made in the periphery of the cornea and two thin arcs of polymathy methacrylate are pushed in between the layers of the stroma on either side of the pupil before the incision is closed. The segments then push out against the curvature of the cornea, flattening the peak of the cone and returning it to a more natural shape. The procedure, carried out on an outpatient basis under local anesthetic, offers the benefit of being reversible and even potentially exchangeable as it involves no removal of eye tissue.

The principal intrastromal ring available is known by the trade name Intacs, Ferrara or Kera rings. Intacs are ring segments and are hexagonal in cut section and are placed outside the optical zone, whereas the smaller prismatic Ferrara ring segments are placed just inside the 5 mm optical zone. In common with penetrating keratoplasty, the requirement for some vision correction in the form of spectacles or contact lenses may remain subsequent to the operation. Potential complications of intrastromal rings include accidental penetration through to the anterior chamber when forming the channel, postoperative infection of the cornea, and migration or extrusion of the segments.
Earlier TG-PRK and more recently TG-ASA is used in treatment of keratoconus suspect patients or in borderline keratoconus patients for stabilization of disease and correction of glasses. It may be done in more advanced keratoconus also in combination with other procedures to improve vision and create a more regular corneal curvature. link
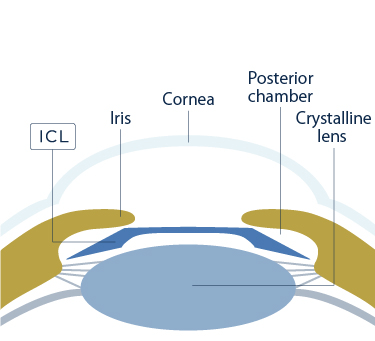
ICL or Toric-ICL / IPCL is being used for correction of refractive errors (glasses) in keratoconus patients. A toric ICL may be performed in addition to the C3R procedure which aims to stabilize the refractive error.
For details see under
Only certified ICL Eye Hospital in the region