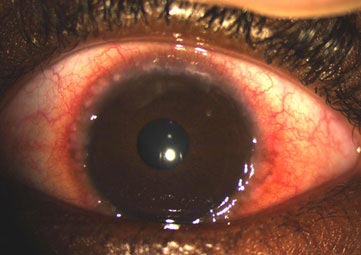
Allergic conjunctivitis (Vernal Catarrh, Spring Catarrh) is caused by airborne allergens (eg.pollen, dust etc.) contacting the eye,. It typically presents as bilateral ocular pruritus (itching), redness, and watery discharge. It may be perennial (all year round) or seasonal (SAC) in spring or pollen season.

Antihistamine / Vasoconstrictor combination products(nephazoline and phenaramine), antihistamines with mast cell stabilizing properties (olopatadine), mast cell stabilizers(cromolyn sodium) and, for refractory symptoms, topical glucocorticoids .
Mast cell stabilizing agents include cromolyn sodium. Full efficacy is reached 5 to 14 days after therapy has been initiated and therefore these medicines are not useful for acute symptoms .
Topical glucocorticoid (steroid eye drops) preparations may be considered in patients with refractory symptoms. Topical glucocorticoids should only be used for short "pulse therapy" of two weeks maximal duration in patients for whom antihistamines with mast cell stabilizing properties have not controlled symptoms adequately. Ocular side effects from glucocorticoids can be vision threatening and include cataract formation, elevated intraocular pressure (IOP), glaucoma, and secondary infections.
Dry eye can coexist with allergic conjunctivitis and worsen it through two mechanisms.
Signs and symptoms include discharge, redness, watering , foreign body sensation, grittiness, matting (sticking) of eye lashes
Discharge from the eyes is more purulent (pus like) in bacterial conjunctivitis than in viral conjunctivitis (clear watery).
Treatment
