Diabetes Mellitus (Sugar disease) is a common community health problem. From an estimated 30 million patients in India alone in year 2000, the figure increased to 62 million (6.2 crore) cases by the year 2011 and is expected to cross 100 million by the year 2030. The risk of blindness is about 25 times more in a diabetic patient than of a same age non-diabetic patient. Since there is no pain or redness in the eye, the diabetic patient is mostly unaware of the complications developing inside the eye till suddenly he/she notices a marked loss of vision.
The three most affected tissues are those of the kidney (nephropathy), nerves (neuropathy) and the retina (parda) of the eye (retinopathy). When all three complications occur in the same patient it is called diabetic triopathy.
Sight threatening complications occur in a large number of diabetics and these if not diagnosed and treated in time can lead to permanent blindness.
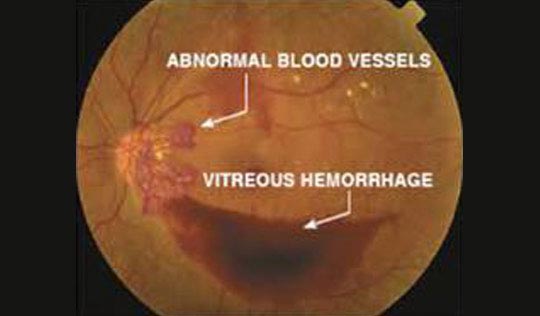
This is one of the most serious eye complications of diabetes. It causes swelling and bleeding in the Retina (Parda) of the eye along with growth of abnormal new blood vessels which cause more complications. The damage is frequently permanent and hence needs prompt treatment. About one-fifth (20%) of all adults found to diabetic for the first time have already developed this complication.
By twenty years of the disease nearly 100% of patients with Type I diabetes (childhood onset type) and 60% of Type II diabetes (adult onset type) have developed this complication
1. The stage of disease before neo-vascularisation has occurred is called “Background Retinopathy” or BDR / Non-Proliferative Diabetic Retinopathy or NPDR.
There can be extensive visual loss in this stage also, in case of swelling of the centre of the retina (Macular Edema, CSME) .Fine blood vessels that leak fluids and lipids in centre of retina to form hard exudates thereby causing vision loss .
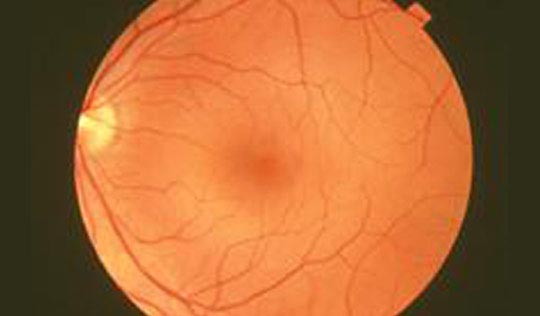 NORMAL RETINA PHOTO
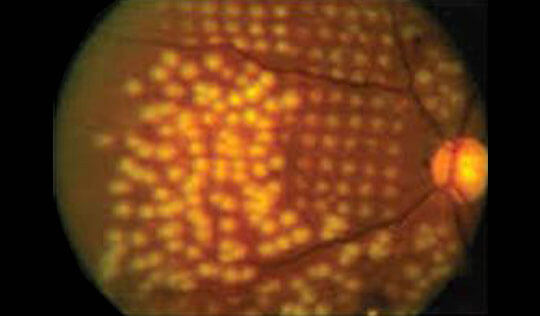
NORMAL RETINA PHOTO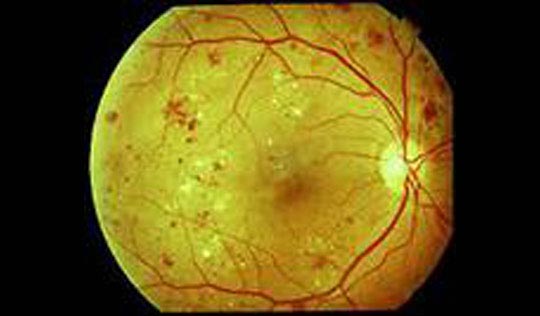 NPDR
NPDR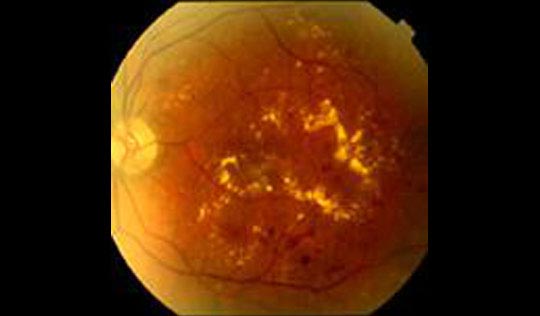 NPDR with CSME
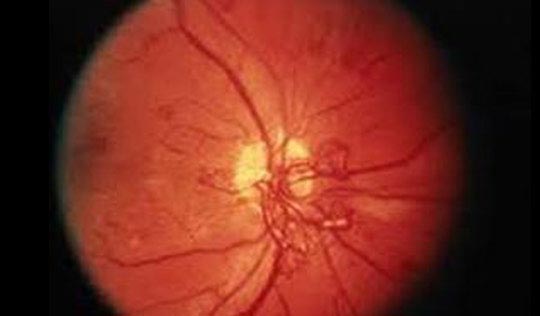
NPDR with CSME2. Once neo-vascularisation (formation of new abnormal blood vessels) has developed the disease is said to have entered the stage of “Proliferative diabetic Retinopathy” or PDR. The risk of sudden visual loss due to bleeding from new abnormal fragile retinal vessels inside the eye (pre-retinal or vitreous hemorrhage) is quite high in this stage.These abnormal blood vessels grow scar like tissue with them which may pull the retina away causing tractional Retinal detachment .
There are three major treatments for diabetic retinopathy, which are very effective in reducing vision loss from this disease.
Diabetic retinopathy is detected during an eye examination that includes:
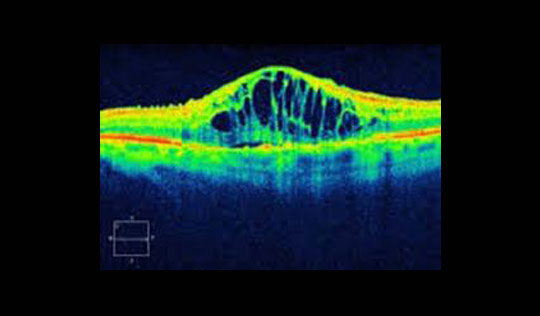
If macular edema is suspected, FFA and sometimes OCT may be performed.

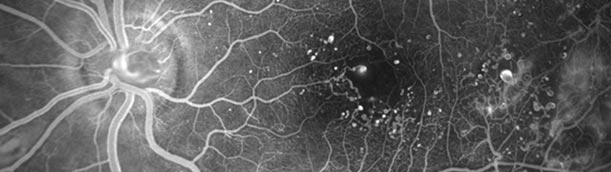
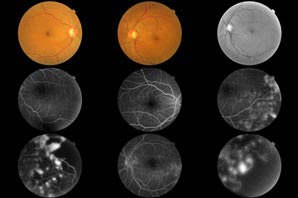
Fundus fluorescein images
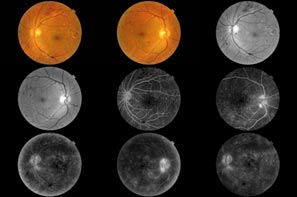
This produces an optical cross sectional images of the retina which can be used to measure the thickness of the retina and to resolve and analyze its major layers, allowing the observation of swelling.
Laser or other Diabetic Retinopathy treatment is undertaken after fundus test and other advanced tests available here like the latest Spectral OCT-SLO (that is OCT Optical Coherence Tomography) with (SLO Scanning Laser Ophthalmoscope).
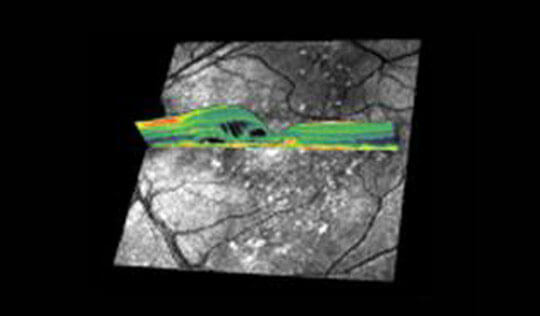
SPECTRAL OCT - SLO IMAGES
To confirm diagnosis, to know the extent of damage ,to plan treatment schedule and to record various changes for future reference we suggest a fluorescein angiogram and OCT.
Laser machines emit a special type of laser light beam (infrared or green / yellow) which helps to coagulate or seal any bleeding or leaking blood vessels in the retina along with destroying any abnormal vessel growth, reducing swelling etc. As and when diabetic retinopathy progresses, further sessions of laser photocoagulation may be required.
Laser Photocoagulation can be used toPanretinal Photocoagulation reduces the contrast. The night vision is reduced and hampers with driving at night. For patient with Diabetic Maculopathy, the Laser treatment reduces the central vision and may affect the quality of vision. Although, in long term it prevents loss of vision.
Multispot, ultrafast,Precise , micropulse, painless Green or Yellow PASCAL LASER is the latest advancement in this field and it was started for the first time in North India at Grover Eye Laser Hospital.PASCAL is a TECHNOLOGICAL BREAKTHROUGH IN PHOTOCOAGULATION LASERS Multi-spot, ultra-fast & safe for Focal or PRP retinal photocoagulation. Delivering a precise pre-set pattern of up-to 56 spots in one shot PASCAL has revolutionized retinal laser treatment. Pascal Laser compensates the patient by being safer, painless, precise and faster and thus the patient tolerates more laser spots in one sitting and hence needs less laser sittings and less repeat visits to the doctor. One or two Pascal sittings are enough for most patients as opposed to 3 to 4 or at times even more sittings needed with older green or red laser.

PASCAL LASER
PAINLESS, PRECISE, PATTERN SCAN LASER – PASCAL – was installed at Grover Eye Laser & E.N.T. Hospital, the first such laser in entire North India.


In addition to Pascal laser the use of latest anti-VEGF medication / intra-vitreal injections like Avastin, Macugen or Lucentis / Accentrix at Grover Eye Laser Hospital have made a world of a difference to the treatment of many eye diseases.
Certain new medicines (Anti-VEGF / intra-vitreal injections) like Avastin, Macugen, Accentrix, Lucentis, IVTA & Ozurdex implant etc. are at times used to control leaking blood vessels (neovascularisation) and swelling inside the eye (macular edema). These are given as injections directly inside the eye with all aseptic precautions. People with tendency of brain stroke need special care. All these treatments do not guarantee that diabetic retinopathy can be cured, it can only try to minimize the complications and save at least some useful vision in patients who if left untreated are at a very high risk of going permanently blind.
Intravitreal anti-VEGF drugs eg. Avastin, Lucentis, Accentrix -There are good results from multiple doses of intravitreal injections of anti-VEGF drugs . Present recommended treatment for diabetic macular edema is Modified Grid laser photocoagulation combined with multiple injections of anti-VEGF drugs.
Triamcinolone is a long acting steroid preparation. When injected in the vitreous cavity, it decreases the macular edema (thickening of the retina at the macula) caused due to diabetic maculopathy, and results in an increase in visual acuity. The effect of triamcinolone is transient, lasting up to three months, which necessitates repeated injections for maintaining the beneficial effect. Complications of intravitreal injection of triamcinolone include cataract, steroid-induced glaucoma and endophthalmitis.
A vitrectomy is performed when there is a lot of blood in the vitreous. It involves removing the cloudy vitreous and replacing it with a saline solution.
If the bleeding inside the eye is too extensive for direct laser treatment and the same does not clear off on its own within a few months, the blood and fluid inside the eye have to be removed by the major operation of vitrectomy and endolaser. Vitreo-Retinal surgery with endo-laser & silicone oil injection is done in cases of TRD (tractional retinal detachment).
Vitrectomy is frequently combined with other modalities of treatment.
Use of PASCAL Laser treatment and latest anti-VEGF medication / intra-vitreal injections like Avastin, Macugen or Lucentis / Accentrix at Grover Eye Laser Hospital have made a world of a difference to the treatment of diabetic retinopathy.Surgical treatment of diabetic treatment is done by vitreoretinaL surgeon .

As explained above, like diabetes itself, once developed diabetic retinopathy can never be totally cured, so prevention plays a very important role. A thorough check-up by an eye specialist at the time of diagnosis of diabetes and regular intervals subsequently aids in timely detection and prompt treatment of complications as and when they occur. All diabetic patients should have regular eye tests (every 6 months / yearly) by a retina specialist even if they do not feel any eye problem of their own. Those who have developed diabetic retinopathy may need more frequent check-ups
Though the duration of diabetes has a strong bearing on the occurrence of this complication (and this unfortunately increases with every year of having diabetes), a strict metabolic control in consultation with the medical specialist / diabetologist is very important.
To minimize further progression of the retinopathy it is very important to control blood sugar (including HbA1c), Lipid Profile (Cholestrol, Triglycerides etc.) & High B.P. Cigarette smoking, tobacco or alcohol abuse and concurrent kidney disease (tested by KFT, urea, creatinine & micro-albumin in urine) increase the severity of the disease and thus should be taken care of.
All people with diabetes - both type 1 and type 2 - are at risk. That's why everyone with diabetes should get a comprehensive dilated eye examination at least once a year. The longer someone has diabetes, the more likely he or she will get diabetic retinopathy.
To confirm diagnosis, to know the extent of damage ,to plan treatment schedule and to record various changes for future reference we may suggest a fluorescein angiogram and OCT.
Non proliferative diabetic retinopathy is characterized by Intra retinal Hemorrhages with or without swelling of Macula.
Proliferative retinopathy is characterized by the growth of new abnormal blood vessels on the surface of the retina, which may lead to vitreous hemorrhage and retinal detachment.
For a definitive diagnosis, you may need to undergo a test called a fluorescein angiography. In this test, illuminated dye is injected into the body through your veins (IV). As your blood flows, the dye gradually appears in the retina. Your ophthalmologist will photograph the retina and evaluate its appearance.
Diabetic retinopathy is detected during a comprehensive eye exam that includes:
To confirm diagnosis, to know the extent of damage ,to plan treatment schedule and to record various changes for future reference we may suggest a fluorescein angiogram and OCT.
A diabetic is also more likely to develop sudden vision loss due to occlusion of the retinal vessels (branch or central retinal vein occlusion), bleeding in the vitreous cavity, detachment of the retina, or infections of the cornea and vitreous.
The aim of treatment by laser photocoagulation is to convert hypoxic areas to anoxic areas.
The indications for treatment depend on extent of severity of the disease.
If there are new blood vessels growing, then the eye is divided into four quadrants and a complete PRP i.e. four sittings of Laser are done spanning over a week to ten days. Initial treatment involves the placement of about 2000 - 3000 burns in scatter pattern, extending from the posterior fundus to cover the peripheral retina in multiple sessions .
The aim of treatment by laser photocoagulation is to induce involution of new vessels and prevent recurrent vitreous haemorrhage
LEADING RETINA HOSPITALS OF THE WORLD HAVE SWITCHED OVER TO PASCAL LASER FOR TREATMENT OF THEIR PATIENTS.
Though being costlier than earlier lasers it compensates the patient by being safer, painless ,precise and faster and thus the patient tolerates more laser spots in one sitting and hence needs less laser sittings and less repeat visits to the doctor .One or two Pascal sittings are enough for most patients as opposed to 4 to 6 or at times even more sittings needed with older lasers .
Major complications like vitreous haemorrahge and Retinal detachment can occur in some patients .Some people develop a condition called macular edema. It occurs when the damaged blood vessels leak fluid and lipids onto the macula, the part of the retina that lets us see detail. The fluid makes the macula swell, which blurs vision.
As explained above, diabetic retinopathy can never be totally cured, so prevention plays a very important role. Though the duration of diabetes has a strong bearing on the occurrence of this complication (and this unfortunately increases with every year of having diabetes), a strict metabolic control in consultation with the medical specialist / diabetologist is very important. Cigarette smoking, abnormal Lipid Profile, High B.P. (hypertension) and concurrent kidney disease (tested by KFT & micro-albumin in urine) increase the severity of the disease and thus should be taken care of.