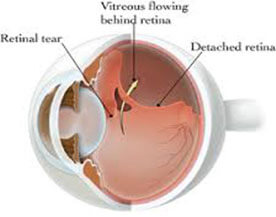
Retina is the light sensitive cells and nerve layer at the back of the eye that senses light and sends images to the brain. It is commonly called "parda" in North India.
WHAT IS THE VITREOUS?Vitreous is the jelly-like material that fills most of the space inside the eye. As we age, the vitreous often liquefies. This is more likely to occur in eyes that are nearsighted (myopia). It can also occur after injuries to the eye or inflammation in the eye.
WHAT IS RETINAL DETACHMENT ?The retina is attached to the inner back surface of the eye. Detachment is the pulling away of the retina from its normal position. The separation of the retina from the wall of the eye impairs its normal functioning, resulting in blurred vision.
 RETINAL DETACHMENT
RETINAL DETACHMENT
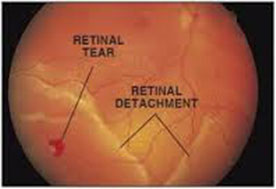
The vitreous is a clear gel that fills most of the space in the eye. It is located in front of the retina. With age, the vitreous pulls away from its attachments to the retina, usually without causing problems. Sometimes the vitreous pulls hard enough to tear the retina. Fluid may then pass through the retinal tear and lift the retina off the wall of the eye.
The retina is examined with an instrument called the indirect ophthalmoscope after dilating the pupil. Holes and tears are carefully looked for in the periphery of the retina.
Indirect Ophthalmoscopy for Peripheral Retinal Examination

Pascal Laser Retinopexy around the hole
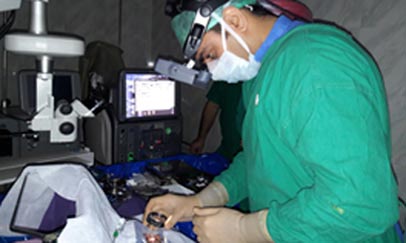
Requires surgery as soon as possible to put the retina back in its proper position. The longer the retina stays detached, the less the visual improvement after surgery.
1. Scleral buckle surgeryA flexible silicone band is placed around the eye to counter the force pulling on the retina after removing the fluid under the detached retina. Like a belt holding up a fat man's pants by tightening it at the waist.
The vitreous gel pulling the retina is removed from the eye and replaced with a special gas or silicone oil. We have all advanced equipment including endo-laser and trained doctors for this at our hospital.

Complicated RD

Vitreo Retinal Surgery
The more severe the retinal detachment and the longer its duration, the less is the visual improvement after surgery. For this reason it is very important to see an ophthalmologist at the first sign of any trouble. If the condition is left untreated it results in loss of useful vision.
A retinal detachment is a separation of the Neurosensory layer from Retinal Pigment Epithelium.
Most retinal detachments are a result of a retinal break either hole, or tear.
Flashing lights and floaters
shadow or curtain that affects any part of the vision
Decreased Vision
Younger adults (25 to 50 years of age) who are highly nearsighted (myopic)
Associated with peripheral retinal degeneration
Older people following Cataract surgery
Trauma
Blunt trauma, as from a tennis ball or fist Penetrating injury by a sharp object A family history of a detached retina In as many as 5% of patients with a non-traumatic retinal detachment of one eye, a detachment subsequently occurs in the other eye. Accordingly, the second eye of a patient with a retinal detachment must be examined thoroughly and followed closely, both by the patient and the ophthalmologist .Diabetes can lead to a type of retinal detachment that is caused by pulling on the retina (traction) alone, without a tear.
Retinal detachment can be prevented by doing prophylactic barrage laser. Barrage laser is indicated in following conditions
A tear or hole of the retina that leads to a peripheral retinal detachment causes the loss of side (peripheral) vision.
Almost all of these patients will progress to a full retinal detachment and loss of all vision if the problem is not repaired.
Early diagnosis and repair are urgent since visual improvement is much greater when the retina is repaired before macula or central area is detached.
Floaters appear as gray or black specks, lines, or "cobwebs", worms, rings or dots in front of the eyes. As the eyes move, the floaters move too. They do not follow your eye movements precisely, as they usually drift when the eyes start or stop moving. Floaters are caused by clumping of pre-existing vitreous fibers in the eye or bits of material suspended in the vitreous jelly that fills the back of the eye.
The floaters cast shadows on the light sensitive retina. It is actually the shadow of the floater that you see. Floaters may have a variety of causes, some serious, and some not serious at all. Some floaters are red blood cells or blood clots on the surface of the retina or floating in the vitreous. Such blood cells may occur with some retinal tears but do not necessarily indicate a tear. Occasionally, the vitreous can pull on a blood vessel on the surface of the retina and cause bleeding without causing a tear of the retina. Vascular disorders such as diabetic retinopathy and vein occlusion frequently result in bleeding inside the eye.
Rarely, floaters may be inflammatory in origin. Diseases such as pars planitis and uveitis can cause the formation of clumps of white blood cells (cells that the body produces when there is inflammation).
Flashes are sensations of light, when no light is really there. They may appear as many tiny bright lights (like "sparklers") or like flashes of lightning.
Flashes occur when the vitreous jelly pulls on or tears the retina. These flashes usually last for only a second or so, but typically occur repeatedly. They may be more obvious with eye movement or in a dark room.
Other causes of flashesSome people with migraine headaches may experience a different type of flash. These are usually shimmering, jagged lights that are present constantly for a period of ten-fifteen minutes or so. They typically appear in the center of your field of vision, and progress slowly towards the edges of the visual field. A headache that is commonly throbbing, and on one side of the head, may follow the disappearance of the flashes.
Low blood pressure can cause people to see stars or specks of light, particularly if they change position quickly. An example would be standing quickly from a sitting position or rising quickly after stooping or bending over. Pregnancy related high blood pressure (pre-eclampsia) could also cause light flashes.
Many people have floaters. This happens in over 70% of the population as part of the normal aging process. Floaters that you have had for years, and that show little change, are usually not serious. It is the sudden onset of one or more new floaters that may be serious. The onset of flashes may also be serious.
Anyone with flashes or the sudden onset of a new floater (or floaters) needs a dilated fundus examination (looking at the vitreous and retina with specialized equipment after putting dilating eye drops to enlarge the pupils).
CAN FLASHES AND FLOATERS CAUSE TOTAL BLINDNESS?Not of their own, floaters cause only a slight blockage of the vision at worst and are usually not detectable by visual testing unless they are very severe.
Importantly, floaters can be related to retinal detachment or a variety of vascular conditions such as diabetic retinopathy, while flashes can be related to retinal tears (breaks) or detachment. They may be a symptom of Retinal Detachment which can lead to blindness if not treated in time.
WHAT CAN BE DONE ABOUT MY FLOATERS AND FLASHES?Your flashes are likely to go away on their own within a few days to weeks. This may be true even if you have a retinal tear or detachment! It is therefore important to be examined by an ophthalmologist even if your flashes go away on their own.
Floaters tend to last longer than flashes. If the floaters are due to blood cells, they will typically disappear.
Most floaters are condensed vitreous collagen fibers and never completely disappear.
There is no medicine, eye drop, vitamin, herb, or diet that is beneficial to patients with flashes or floaters. However if a retinal hole or tear is present it must be treated.
If light flashes are due to a posterior vitreous separation only (PVD) and no retinal breaks (tears) are found on careful examination with the pupil dilated, no treatment is necessary. If the doctor finds tears, laser or occasionally freezing (cryo) treatment is needed.
If you have a retinal detachment, your doctor will talk to you about the treatment. We have the world’s best PASCAL laser, endo-laser, trans-scleral laser and advanced vitreo-retinal surgery equipment and expertise to treat this condition.