WHAT IS GLAUCOMA
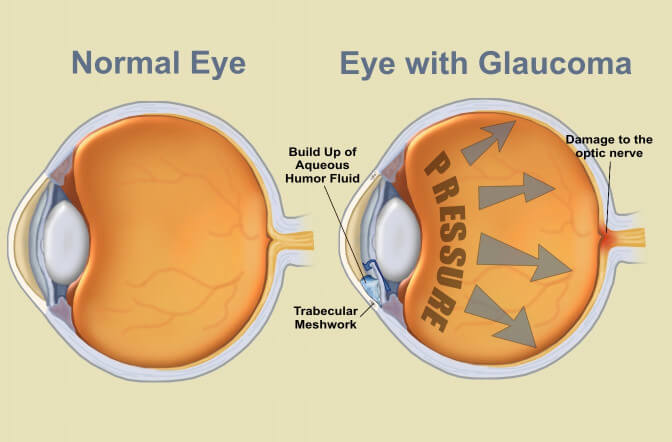
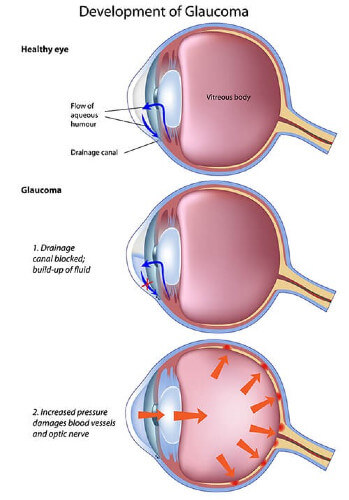
A clear fluid called the Aqueous humor circulates continuously within the eye. Produced behind the iris, it flows forwards through the pupil and drains out of the eye through a meshwork of drainage channels. The amount of fluid produced inside the eye, balances the amount of fluid that flows out of the eye thereby keeping pressure within the safe range. Glaucoma (KALA-MOTIA) is a group of disorders wherein the pressure of the fluid inside the eye, called Intraocular Pressure (IOP*) rises to such a level that it damages the delicate structures of the eye specially the nerve of sight (Optic Nerve).
Glaucoma is now understood to be a condition with compromised blood flow (perfusion) to the eye and it’s nerve wherein the eye pressure is an important but not the only variable.
Average Intra-Ocular Pressure (IOP) in adults is 16mmHg. The range varies from 9mmHg to 21mmHg. If the pressure is consistently above 21mmHg, the chances of eye damage are probably around ten percent. When the pressure is above 26 mmHg, the likelihood increases to about fifty percent. If the IOP persists above 30 mmHg, the damage will definitely occur.
Glaucoma is called the Silent thief of sight as the disease may damage 80% of the optic nerve (nerve of sight) before a person realizes the effect on vision. A person with Chronic Glaucoma is usually unaware of the disease. On the other hand, Acute Glaucoma, in which the pressure rises rapidly, causes severe symptoms that force the patient to consult a doctor.
Some symptoms which may be suggestive of Glaucoma are:

Misty Morning a Lovely Sight, but Foggy Viion a Dreadful Fright
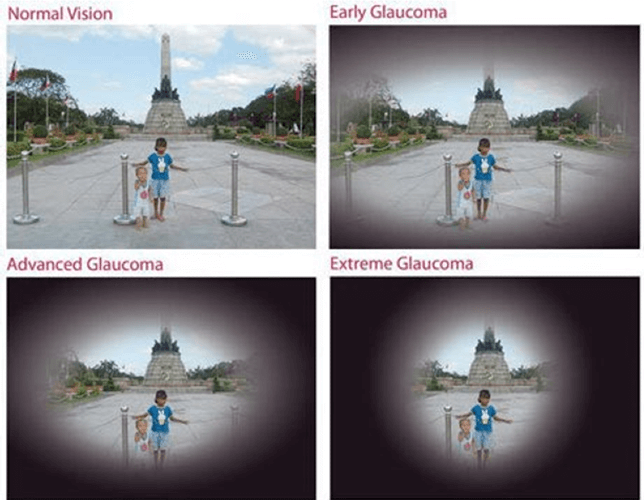
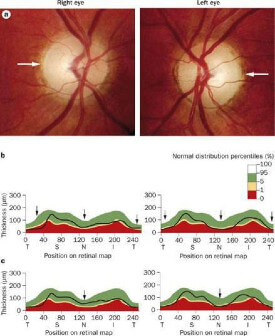
Progressive Vision Loss, Visual Field Constriction in Glaucoma
The eye does not see what the mind does not know. Our doctors are trained in the best institutions and coupled with vast experience and advanced facilities in our hospital they are likely to diagnose glaucoma earlier & to treat it earlier to save you from later problems.
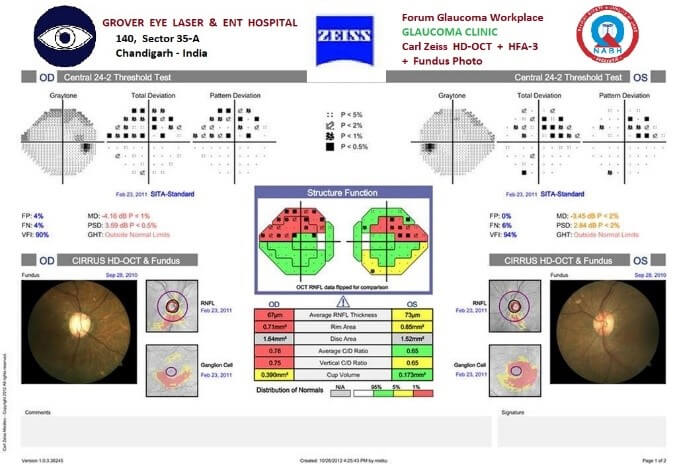
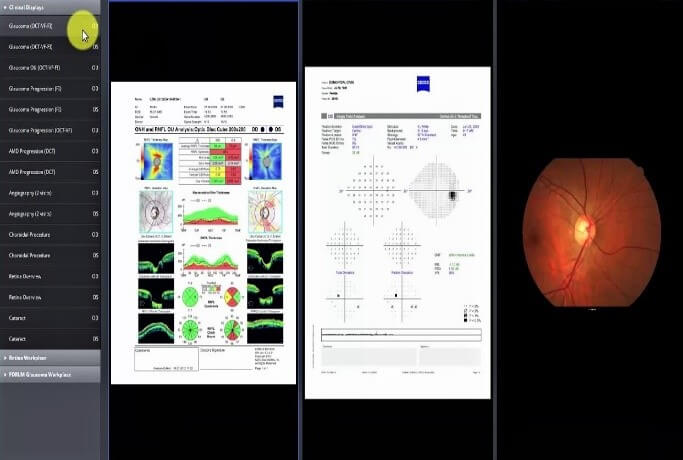
FORUM : Combined Glaucoma Eye Structure & Function Analysis reporting system at our Hospital.
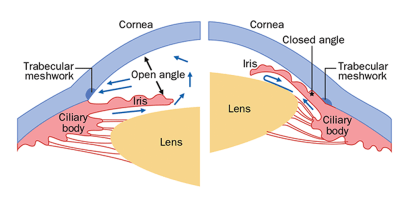
Showing Open and Closed Angles
In open-angle glaucoma, the drainage angle of the eye is open on Gonioscopy Test. The eye aqueous fluid drainage canals are not functional further down. Most people have no symptoms and no early warning signs.
Many patients confuse this gradual painless vision loss with eye sight blurring due to cataract which also causes a painless gradual decrease in vision. But in this case delay in glaucoma treatment causes permanent damage.
In this type of glaucoma the angle of entrance to the drainage canals is very narrow or closed on Gonioscopy Test. In initial stages the angle may open and close intermittently and the IOP, eye pressure rise frequently occurs in episodes (Intermittent ACG) which later becomes permanent as the angle closes completely. This type of glaucoma is quite common in North India.
The more common notion that 'Kala Motia' is accompanied by pain is at times seen in the “Acute” variety of this variant. This type of glaucoma is more common in people needing plus numbered glasses for distance also (hypermetropia). It is also frequently symptomless in initial stages. Some symptoms are as below :
Can be due to many reasons some of which are
This is due to various types of birth defects. These children usually have visible symptoms, such as big cloudy eyes, sensitivity to light, and excessive tearing. It needs to be operated surgically at the earliest. Juvenile glaucoma occurs in later childhood.
5. Normal or Low Tension Glaucoma (NTG / LTG) and Ocular Hypertension
As the very name suggests, in this case the eye pressure (IOP) alone may be misleading. In NTG / LTG, Low Blood Pressure (Low diastolic BP) especially while sleeping at night greatly aggravates the eye damage due to improper blood supply (perfusion) to the eye and the optic nerve repeatedly for some hours every night. This paradoxically can also occur in people with high BP during day but with low B.P. during sleep. Ocular Hypertension conversely means high IOP. without overt clinical signs of glaucoma (this may mean pre-glaucoma in some or just due to thick cornea in others).
(i) Increase of fluid pressure inside the eye (IOP test) resulting in
(ii) Damage to the Optic Nerve (Disc cupping seen on Optic Disc fundus test) which is manifested as
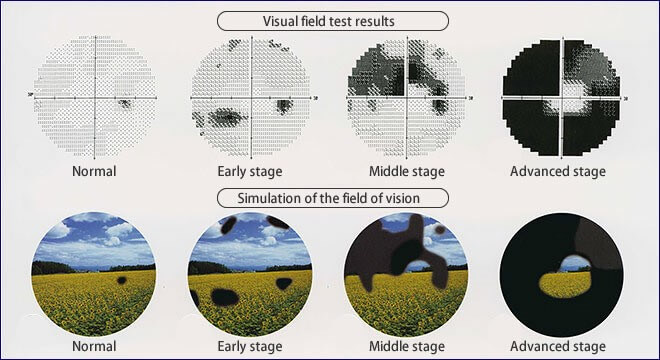
(iii) Loss or constriction of field of vision (Tested by Perimetry / HVF )
(iv) Field loss is due to Retinal Nerve Fiber Layer (RNFL, OCT test) thinning in the presence of
(v) Open or Narrow anterior Chamber Angles of fluid drainage with or without other associated anomalies (checked on Gonioscopy Test).
This sequence forms the logic or basis of the various tests for a glaucoma patient
There are three key features of Glaucoma:
Regular and complete eye exams at Grover Eye Hospital is the key for early detection of glaucoma to protect your vision from damage caused by glaucoma. During a complete work up for Glaucoma, we measure the Intraocular Pressure (Tonometry), the central corneal thickness (Pachymetry), inspect the drainage angle of the eye (Gonioscopy), evaluate for optic nerve head damage (Ophthalmoscopy), test the visual field of each eye (Perimetry), and evaluate for retinal nerve fibre layer (OCT).
To measure the fluid pressure inside the eye by various types of tonometers like Schiotz (metallic scale type), Goldmann Applanation (prism with blue light) or the Computerized Non Contact NCT type which measure pressure with a gentle puff of air without actually touching the eye.

APPLANATION TONOMETRY FOR IOP MEASUREMENT

NON CONTACT TONOMETRY FOR IOP MEASUREMENT
It helps the doctor look at the shape and color of the optic nerve.To check for the Cupping or Atrophy (damage) of the Optic Nerve due to the drying up of the nerve of sight it suffers damage due to high pressure inside the eye.
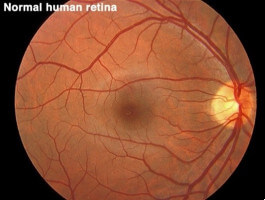
FUNDUS TEST ( OPHTHALMOSCOPY )
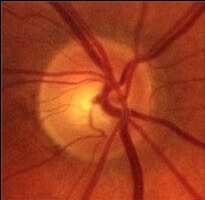
FUNDUS : NORMAL OPTIC DISC
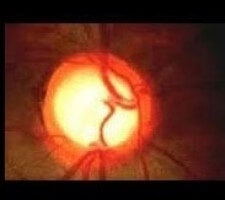
ADVANCED GLAUCOMA CUPPING
Visual Field defects are missing areas in the field of sight, though the person may be seeing well otherwise.This is due to some but not all fibers of the Optic Nerve being damaged at a point of time. This is measured with an instrument called Perimeter.
The modern automated perimeters are computerized to measure and to a great extent evaluate, self-analyze, compare and report the defects or missing areas in the field of vision.Visual Field / Perimetry test also helps to confirm the response to treatment or to diagnose progression of glaucoma.

OCTOPUS PERIMETER
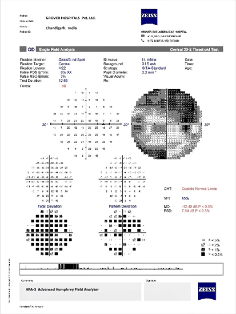

HUMPHERY ZEISS PERIMETER

Automated Perimetry is a procedure where the patient wears a patch over one eye and looks straight ahead at a fixation point inside a white bowl shaped equipment. At the same time, the computer presents lights in variable intensity and variable locations inside the bowl. The patient presses a button each time he or she sees the light, which is why perimetry can provide a map of the visual fields. The type of vision loss associated with glaucoma is relatively specific, and perimetry can detect the typical visual-field defects of glaucoma . This test can also pick up vision problems due to various other nerve or neurological (brain) disorders also.
The slow death of nerve fibers is the earliest damage to occur in Glaucoma. This nerve fiber layer damage is picked by an instrument called OCT.
Spectral Optical Coherence Tomography (SD OCT, HD OCT ) with Scanning Laser Ophthalmoscope (SLO) is an advanced spectral laser scan of the anterior segment, retina and optic nerve head done at our hospital. Retinal Nerve Fiber Analysis / OCT-RNFL analysis is a advanced method of glaucoma testing in which the thickness of the nerve fiber layer is measured and the OCT machine produces a contour map of the optic nerve head, optic cup and measures the retinal nerve fiber thickness. Thinner areas may indicate damage caused by glaucoma. This test is especially suitable for patients who may be considered to be glaucoma suspect and also to indicate if a person’s glaucoma is progressively becoming worse or is stable.


Retinal Nerve Fiber Analysis / OCT-RNFL analysis
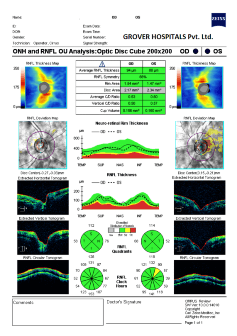
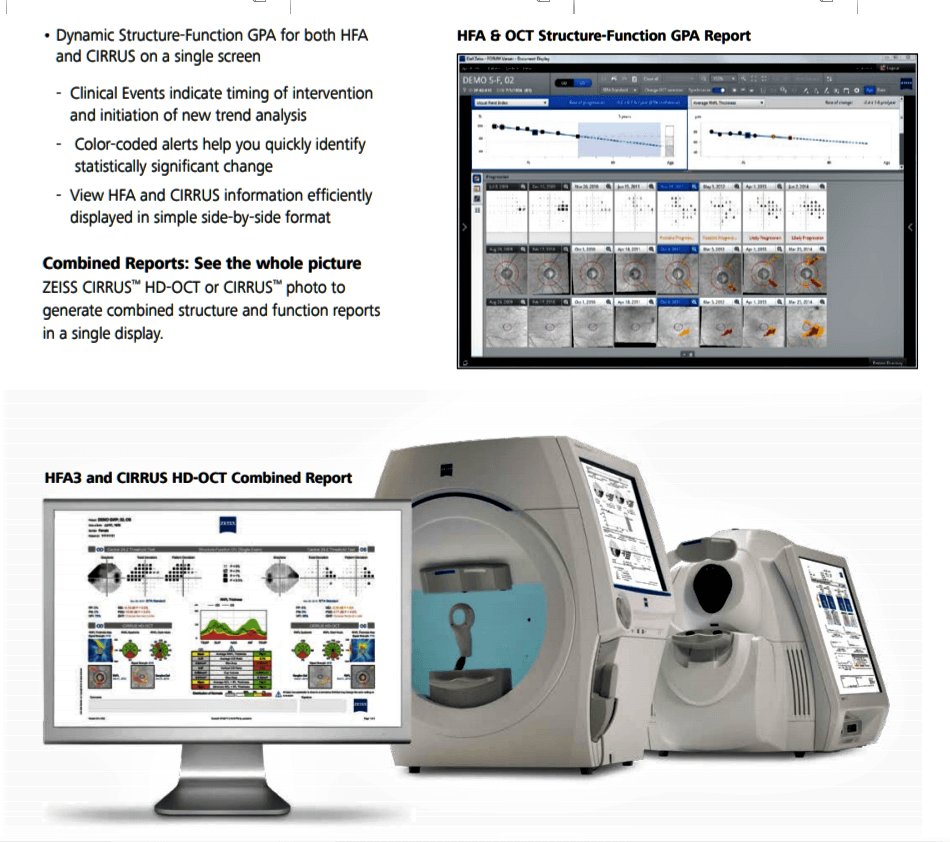
FORUM : Combined Glaucoma Eye Structure & Function Analysis reporting system at our Hospital.
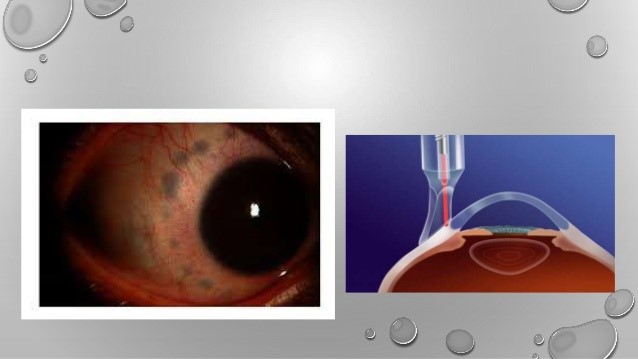
Gonioscopy test is used to observe the anterior chamber angle or the drainage points of the eye.


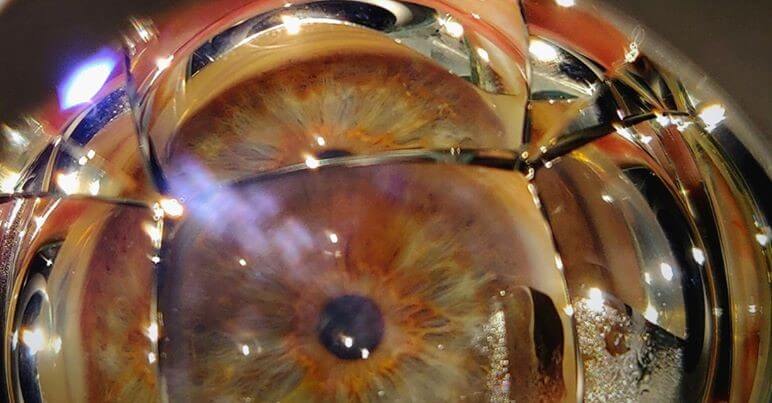
It is done to detect whether anterior chamber angle is open or narrow. Once the surface of the eye has been numbed with eye drops, eye specialist will place a special contact lens on your eye. This lens will allow eye specialist to see the eye’s drainage system and check if the angle where the iris meets the cornea is open or closed.
We have also installed DIGS Pro the digital smart imaging system to screen for angle closure suspects in a slit-lamp-free rapid manner in the times of COVID-19, this risks a long time exposure when done on a slit-lamp.

ULTRASONIC PACHYMETRY
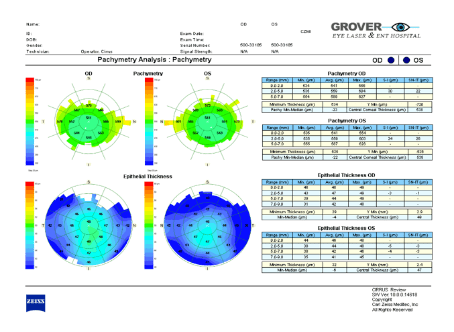
OCT PACHYMETRY PRINT OUT
OCT PACHYMETRY
Pachymetry is the method of measuring the thickness of the cornea and to calculate individual Target IOPLINK Corneal thickness is critical because it can change an accurate reading of eye pressure, causing doctors to treat you for a condition that may not really exist (ocular hypertension) or to under treat you and risk increases glaucoma damage (Low Tension Glaucoma). Actual IOP may be underestimated in patients with thinner CCT (central corneal thickness) and overestimated in patients with thicker CCT. Pachymetry is a simple, quick, painless test. With this measurement doctor can better understand your IOP reading, determine a target IOP and develop a treatment plan that is right for your condition.
The eye pressure (IOP) does not remain the same throughout the day and there may be significant variation throughout the day, with eye pressure being normal at times, and so may be a cause of missed diagnosis at times. DV test is done to check IOP & BP fluctuations over a 24 hour period. Usual time for such recordings is 10am, 2pm, 6pm, 10pm, 2am and 6am. So it is best done only in a hospital with facility for overnight admission.

Triggerfish is a contact lens device for recording IOP throughout the day (Sensimed AG). Approved by the FDA in 2016, the device is capable of recording continuous eye pressure changes over the course of 24 hours.
As explained earlier optic nerve damage (Optic Disc Cupping / Optic Atrophy) and consequent blindness due to glaucoma is irreversible, hence early detection with prompt and regular treatment are the keys to successful glaucoma management. Glaucoma is said to be controlled not cured as treatment can at most halt further damage but generally cannot reverse damage already done.
The aim of treatment is to reduce and to maintain the fluid pressure (IOP) inside the eye to a level at which further optic nerve damage does not occur, called Target IOP .
TARGET IOP for each patient is decided after detailed tests at our hospital. On long term follow up of an individual patient the eye surgeon can be sure of good glaucoma control when IOP remains at an acceptable level at all times and further visual field loss on repeated perimetry (function test) and OCT-RNFL (retinal nerve fiber layer - structure test) does not occur. The generally accepted upper limit of IOP is 20 mmHg. but levels much below this may desirable though there may considerable individual variations.
Whatever may be the approach, the objective of the treatment is generally to lower the eye pressure to a level at which optic nerve damage does not progress or worsen.
Anti-Glaucoma eye drops are the first line of treatment. They act to decrease eye pressure either by reducing the production of aqueous fluid within the eye or by improving the fluid outflow through the drainage channels. Tablets may be required at times. Some medicines occasionally result in allergy or unwanted side effects. Medication should never be stopped or changed without consulting your doctor ophthalmologist.

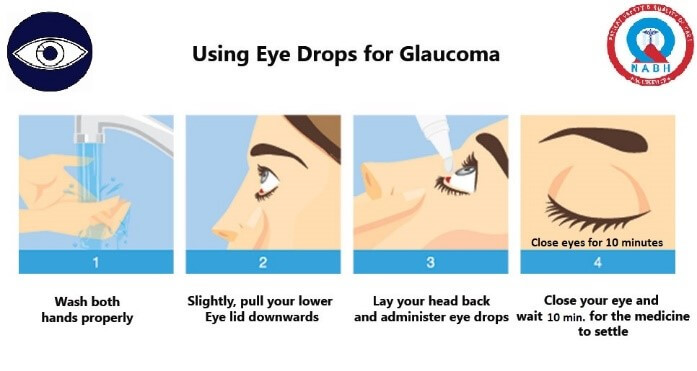
Regular eye examination and glaucoma tests are crucial to monitor any progression of glaucoma despite the glaucoma treatment in a particular patient.
YAG LASER, TSCP, GREEN LASER, SLT LASER, PASCAL & PLT LASER are used in the treatment of Glaucoma.
A. Advanced Q-Switched Nd-YAG Laser is used for LPI / LI - Laser Iridotomy (link) in almost all Narrow Angle Glaucoma cases. In angle-closure Glaucoma, an opening is made in the iris (YAG Laser Iridotomy, LI) to restore the free flow of aqueous fluid and is the initial treatment of choice in these cases.

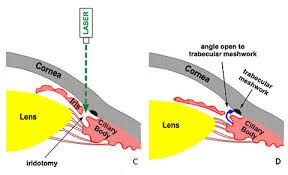

LI - Laser Iridotomy Procedure
B .Selective Laser Trabeculoplasty (SLT) or the more advanced auto Pattern Laser Trabeculoplasty (PLT) with PASCAL Laser (available only at our hospital in the region) is helpful for some cases of Open Angle Glaucoma and also in some Narrow Angle Glaucoma cases after LI. In some cases the drain itself is treated . Laser trabeculoplasty is performed as an OPD procedure. Several evenly spaced Laser burns stretch the drainage holes in the meshwork which impoves the drainage of aqueous fluid .
Laser helps to either stop or reduce the medications to control the pressure. In many cases, glaucoma drugs are required even after this procedure.
i.
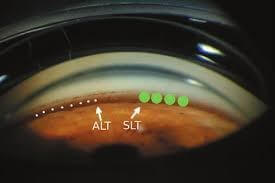
ii.
Diagram illustrating relative sizes of the laser spots and their placement on the trabecular meshwork in various approaches to trabeculoplasty: Laser trabeculoplasty (LT), Selective laser trabeculoplasty (SLT), Micropulse diode laser trabeculoplasty (MDLT), and Patterned laser trabeculoplasty (PLT).
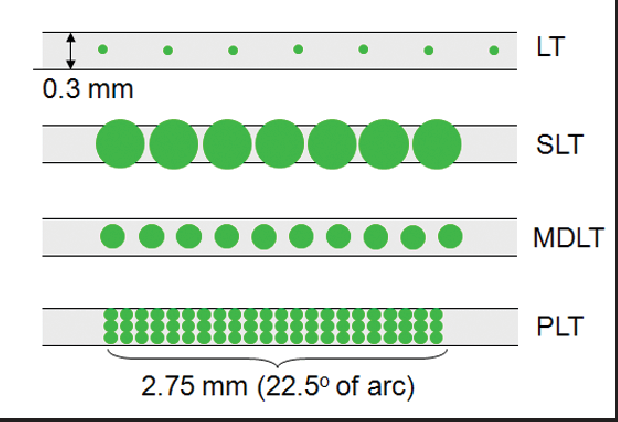

Pattern Laser Trabeculoplasty (PLT)

C. Trans-Scleral Cyclo-Photocoagulation (TSCP Laser), Diode Laser Cyclo-photocoagulation (DLCP) & Cryo Surgery are also available in our most advanced eye operation theatre of the region.
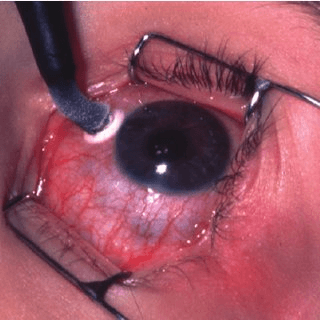
CYCLOCRYO
D LCP
TSCP
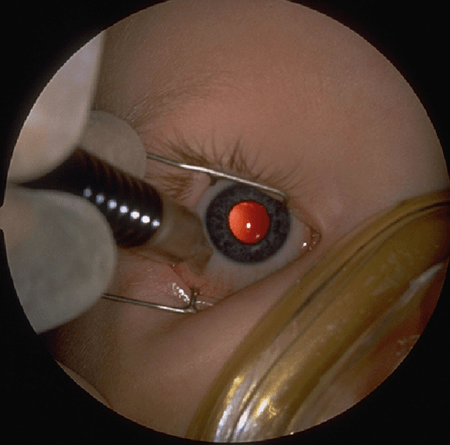
Various types of Glaucoma surgeries done are Trabeculectomy, Trabeculotomy, Goniotomy, Deep sclerectomy, Viscocanalostomy, Endoscopic Cyclophotocoagulation (ECP), Gonioscopy-Assisted Transluminal Trabeculotomy (GATT), Micro (or Minimally) Invasive Glaucoma Surgery (MIGS) etc.
Surgery is done generally to create or open a filtering or fluid drainage channel to control the IOP in Glaucoma. We use miniature instruments to create a new drainage channel for fluid to leave the eye. If needed special adjuvants like 5FU or MMC are used or special Glaucoma shunts / implants / valves / setons may be used. Usually surgery for glaucoma recommended only if the medicines and laser fail to prevent damage or some specific reason. Conventional surgery is about 65 to 80 percent effective at lowering eye pressure.

Showing Trabeculectomy Filtering
Since most of the damage due to glaucoma is not reversible, Early detection, regular treatment and follow-up is is the key to prevent progressive loss of sight from glaucoma. Whatever may be the approach, the objective of the treatment is to lower the eye pressure to a level (Target IOP) at which optic nerve damage does not develop or worsen. A target IOP for a particular patient is determined as per the consultant's assessment.
GROVER EYE LASER HOSPITAL is best equipped for all advanced Glaucoma Tests, Lasers & Surgeries.