An opacity in the natural eye lens present at birth is called a congenital cataract. Some lens opacities do not progress and are visually insignificant (need no treatment), others can produce profound visual impairment and need urgent surgery in an infant as young as 2 to 3 weeks.
Congenital cataracts may be unilateral or bilateral. They can be classified by morphology, presumed or defined genetic etiology, presence of specific metabolic disorders, or associated ocular anomalies or systemic findings.

Congenital Cataract
In general, approximately one-third of congenital cataracts are a component of a more extensive syndrome or disease (e.g., cataract resulting from congenital rubella syndrome), one-third occur as an isolated inherited trait, and one-third result from undetermined causes. Metabolic diseases tend to be more commonly associated with bilateral cataracts.
All newborns should have screening eye examinations, including an evaluation of the red reflexes.
In general, the younger the child, the greater the urgency in removing the cataract, because of the risk of amblyopia (llazy eye). For optimal visual development in newborns and young infants, a visually significant unilateral congenital cataract should be detected and removed before age 6 weeks, and visually significant bilateral congenital cataracts should be removed before age 10 weeks.
Once the cataract is removed, it is absolutely vital that your child's eye be corrected with a surgically implanted lens (intraocular lens), contact lens or eyeglasses. Without vision correction following cataract surgery, the eye will have poor vision, and normal infant eye and brain visual pathway development will be impeded. Generally very thick and heavy aphakic glasses in the range of +14 to +20 are needed in children after cataract surgery and use are less used now a days. In some cases, contact lenses are fitted on the eye's surface (cornea) may be used to help restore vision after the natural lens is removed during cataract surgery.

Post Cataract Surgery
Current state-of-the-art cataract surgery, phacoaspiration removes the cloudy crystalline lens and replaces it with a clear intraocular lens (IOL) to restore vision. Infants generally need much higher powered IOLs with the power rapidly decreasing with age. Children thus often need glasses even after IOL surgery. Multifocal IOLs may be used for slightly older children. The surgery is generally as safe and effective as for adults except that it is usually done under GA (general anesthesia).
Amblyopia eye exercises and regular follow-up are most important after surgery in infants & young children as all the benefits of surgery can be lost if this aspect of a child's treatment is overlooked.Elevated eye intra-ocular pressure (I.O.P.) with onset in the first year of life is called primary congenital or infantile glaucoma is. It occurs in about 1 out of 10,000 births and results in blindness in approximately 10% of cases and reduced vision (worse than 6/12p) in about half of all cases. Primary congenital glaucoma occurs from an increase in the intraocular pressure in the first year of life. The increased intraocular pressure is thought to occur from reduced aqueous outflow at the level of the trabecular meshwork.
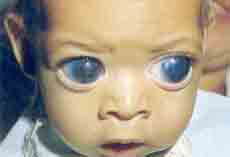
Primary congenital glaucoma typically presents in the neonatal or infantile period with the classic triad of epiphora, photophobia, and blepharospasm in the absence of the discharge that typically accompanies a nasolacrimal duct obstruction or conjunctivitis. Corneal clouding from microcystic edema can occur, accompanied by gradual enlargement of the corneal diameter. Untreated, most cases progress to irreversible corneal opacification, buphthalmos (abnormally large "ox like eye"), and eventual blindness.
The disease is more common in males, typically is bilateral, and does not have a racial or geographic preference. Most cases are sporadic.
The only known risk factors are genetic - consanguinity and affected siblings. The risk of congenital glaucoma in the second child is approximately 5%, and the risk increases to 25% with two affected siblings.
Early detection and urgent treatment are essential to maximize visual potential.
The diagnosis of primary congenital glaucoma can often be made clinically, even without an accurate measurement of intraocular pressure. The hallmark of the disease, however, is an elevated intraocular pressure in the absence of other conditions that can cause glaucoma, such as Axenfeld-Reiger syndrome or aphakia.
The physical exam follows the standard ophthalmology exam for infants and young children. The vision assessment should specifically look for asymmetry in unilateral cases and the presence of nystagmus and/or reduced fixation response in bilateral cases.
Any corneal diameter above 12.5 mm suggests an abnormality, especially if there is asymmetry between the two eyes. A measurement of intraocular pressure may be possible using topical anesthesia in a cooperative child, although an examination under anesthesia (EUA) may be required.
After dilation, a refraction should be performed to look for myopia, astigmatism, and any corneal irregularity. The fundus exam should include a careful exam of the optic nerve to look for asymmetric or large cupping and for any structural abnormalities.
The clinical diagnosis of primary congenital glaucoma can be made by measuring an elevated intraocular pressure in the presence of the clinical signs created by the elevated pressure - corneal edema and enlargement, Haab striae, myopia, astigmatism, and optic nerve cupping.
The main diagnostic test for primary congenital glaucoma is the measurement of the intraocular pressure. In a cooperative infant, this measurement can be obtained in the clinic setting with a Perkins applanation tonometer or a Tonopen. In older patients, standard Goldmann applanation tonometry can be performed.. A newborn has an average intraocular pressure of 10-12 mm Hg, increasing to 14 mm Hg by age 7 or 8 years of age. An asymmetric measurement or an elevated measurement in the presence of other clinical signs helps make the diagnosis of glaucoma.
The management of primary congenital glaucoma is directed toward lowering and controlling the intraocular pressure and treating the secondary complications such as refractive change and amblyopia that develop during the course of the disease.
As opposed to glaucoma treatment in adults wherein eye drops are used first and surgery resorted to later if needed, in congenital glaucoma the mainstay of treatment is surgery. Angle surgery either goniotomy or trabeculotomy, to lower intraocular pressure by improving aqueous outflow. If angle surgery is not successful, filtering surgery trabeculectomy enhanced with mitomycin-C or glaucoma implant surgery with a Molteno, Barveldt, or Ahmed implant can be performed. The most common complication after surgery is poor control of intraocular pressure. The success rate for angle surgery is approximately 80% after 1 or 2 procedures, while the other procedures report a success rate of 33-80%. Doctors at our hospital are well trained and experienced in such surgeries.
Medical therapy for primary congenital glaucoma is typically used as an adjunct to surgery. Oral carbonic anhydrase inhibitors include acetazolamide (10-20 mg/kg/day divided into 3 or 4 doses) Topical carbonic anhydrase inhibitors include dorzolamide 2%, and brinzolamde 1% eye drops TID. Beta-blockers (timolol or equivalent) can also be given topically, usually using a lower starting concentration of 0.25% drops BID. Prostaglandin analogs latanoprost 0.005%, travoprost 0.004% , and bimatoprost 0.03% have been effective in reducing intraocular pressure, although use is discouraged in the presence of inflammatory conditions. The alpha2-adrenergic agonist brimonidine is contraindicated in children under age 2 because of potentially serious lethargy, hypotonia, hypothermia, and CNS depression.
In long term these patients require serial measurements of intraocular pressure, corneal diameter, refractive error, and optic nerve cupping. If an adequate assessment of the clinical response is not possible in the outpatient clinic, an examination under anesthesia can be performed.
The prognosis for primary congenital glaucoma depends on the age of onset. Glaucoma that presents at birth is more difficult to treat, with at least half of the affected eyes becoming legally blind. Likewise, glaucoma that has progressed to create a corneal diameter of 14 mm or more has a similarly poor prognosis. On the other hand, glaucoma that presents from 3-12 months of age has a favorable prognosis, with 80-90% of cases achieving good control of intraocular pressure with angle surgery. Affected children can develop significant myopia from axial elongation of the globe, astigmatism from unequal enlargement of the cornea, corneal scarring, and even dislocation of the lens from excessive anterior segment enlargement. Concurrent or subsequent cataract may also need treatment. Correction of the refractive error and aggressive treatment of associated amblyopia (lazy eye) and/or strabismus is required to maximize visual outcome.
Amblyopia is sometimes called a 'lazy' eye. It is a condition where the vision in an eye is poor and it is caused by lack of use of the eye in early childhood. Amblyopia or 'Lazy Eye' is a condition where the eye is normal to look at, but it just does not work. It usually affects one eye but may be bilateral. It is medically defined as a decrease of visual acuity (sharpness), caused by any form vision deprivation and/or abnormal binocular interaction, that cannot be explained by any disease or disorder in the ocular media or visual pathways (from retina, optic nerve or brain).
Another important feature of amblyopia is that it is a condition caused by abnormal visual stimulation/experience in early childhood during the critical period of visual development. In simpler words, during the early years of development, due to certain forms of stimulus deprivation or abnormal stimuli, the wiring from the eye to the brain gets disrupted or forms abnormal connections with the better eye taking over from the weaker eye and making it lazy.
This plastic period is usually up to 6 -8 years of age and is also the critical period when such process may be reversed or corrected. Hence, the importance of proper eye testing of all pre-verbal and pre-school children by a qualified ophthalmologist who has adequate facilities to test such children.
Amblyopia poses an important socio-economic problem and generally affects 2 to 2.5% of the general population. This in simpler words means that up to 2500 people in a population of one lakh stand to be disqualified from many jobs just because their eyes were not adequately tested or treated in early childhood. This becomes all the more important due to the fact since usually only one eye is involved and the child seems to function normally in school, the parents may not notice anything amiss, and by the time the child himself or herself becomes old enough to realize poor vision it generally is too late.
To understand how amblyopia occurs, it is helpful to understand how vision develops. Newborn babies can see though their focus is not very clear. However, as they grow, the visual pathways continue to develop from the eye to the brain and within the brain. The brain learns how to interpret the signals that come from an eye. This visual development continues until about age 7-8 years. After this time, the visual pathways and the 'seeing' parts of the brain are fully formed and cannot change.
If, for any reason, a young child cannot use one or both eyes normally then vision is not learnt properly. This results in impaired vision (poor visual acuity) called amblyopia. The amblyopia develops in addition to whatever else is affecting the eye. In effect, amblyopia is a problem with the development of vision in the brain, rather than a problem within the eye itself. Even if the other eye problem is treated, the visual impairment from amblyopia usually remains permanent unless it is treated early enough
A squint is the most common cause of amblyopia. In many cases of squint, one eye remains the one that sees (the dominant focusing eye). The other, turned eye (the squinting one) is not used to focusing and the brain ignores the signals from this eye. The turned eye then fails to develop the normal visual pathways in childhood and amblyopia develops in this eye.

Squint Assessment With Glasses
The main treatment for amblyopia is to restrict the use of the good or the better eye. This then forces the affected eye to work. If this is done early enough in childhood, the vision will usually improve, often up to a normal level. In effect, the visual development of the affected eye catches up. The common way this is done is to put a patch over the better eye. This is called eye patching.
The length of treatment with an eye patch is dependent on the age of the child and the severity of the amblyopia. The patch may be worn for a few hours a week or for most of the day, every day. Treatment is continued until either the vision is normal or until no further improvement is found. It may take from several weeks to several months for eye patching to be successful.
Your child will be followed up, usually until about 8 years of age, to make sure that the treated eye is still being used properly and does not become amblyopic again. Sometimes, further patch treatment (maintenance treatment) is needed before the vision pathways in the brain are fixed and cannot be changed.
Occasionally, eye drops to blur the vision in the good eye, or glasses that prevent the good eye from seeing clearly, are used instead of an eye patch.
Vision therapy can be used as a treatment to maintain the good work achieved by eye patching. This involves playing visually demanding games with a child to work the affected eye even harder - like eye training. Expert technicians & doctors at our hospital will guide you for this in addition we have CAM Exercise machine at our hospital for this purpose. CAM eye exercises are usually done for 30 minutes in a session for 10 days in a month on alternate day or daily basis. Eye patching and other treatments for amblyopia aim to improve vision; they do not by themselves correct the appearance of a squint which needs treatment in addition.
1. A squint can be a cosmetic problem. Many older children and adults who did not have their squint treated as a child have reduced self-esteem because of the way their squint looks to other people.
With normal eyes, both eyes look and focus on the same spot. This is called binocular vision (bi- means two and ocular means related to the eye). The brain combines the signals from the two eyes to form a three-dimensional image. If you have a squint, the two eyes focus on different spots. In children with squint this does not usually cause double vision. In children the brain quickly learns to ignore the signals and images coming from the turned (squinting) eye. The child then effectively only sees with one eye. This means the child does not have a good sense of depth when looking at objects. As a result, he or she cannot see properly in three dimensions.
(Adults who develop a squint often have double vision, as their developed brain cannot ignore or suppress the images from one eye.)
It is important to diagnose a squint (and amblyopia) as early as possible. Routine checks to detect eye problems in babies and children are usually done at the newborn examination and at the 6- to 8-week review. There is also a routine preschool or school-entry vision check.
Some newborn babies have a mild intermittent squint that soon goes, reducing by 2 months of age and gone by 4 months of age. However, fixed squints are usually permanent unless treated. So, as a guide:
Various tests can be done to check a child's vision. Sight tests can even be done for babies. Tests to find a squint can involve covering and uncovering each eye in turn. This often shows which eye has the squint and how it moves. The pupils of the eye can be checked with a torch, to check they become smaller (constrict) with light and widen (dilate) when the light is removed. An ophthalmoscope is a special torch used to examine the back of the eye (the retina). Very occasionally, if another cause of squint is suspected (other than a congenital squint or one related to refractive errors), a scan of the eye or the brain may be needed.
Treatment typically involves the following:
If a child has a refractive error (long or short sight, for example) then glasses will be prescribed. This corrects vision in the eye. It may also straighten the squinting eye, if the refractive error was the cause of the squint.
In many cases an operation is advised to make the eyes as straight as possible. The main aim of surgery is to improve the appearance of the eyes. In some cases, surgery may also improve or restore binocular vision (this means that the two eyes are working together).
The exact operation that is done depends on the type and severity of the squint. It may involve moving the place where a muscle attaches to the eyeball or, one of the muscles that moves an eye may be shortened. Sometimes a combination of these techniques is used.

Ptosis is a condition of drooping or falling of the upper eyelid. The sleepy eyes look or drooping may be worse after being awake longer, when the individual's eye muscles are tired. If severe enough and left untreated, the drooping eyelid can cause other conditions, such as amblyopia or astigmatism in young children. This is why it is especially important for this disorder to be treated in children at a young age, before it can interfere with vision development.
Ptosis occurs due to dysfunction of the muscles that raise the eyelid or their nerve supply (oculomotor nerve for levator palpebrae superioris (LPS) and sympathetic nerves for superior tarsal muscle). It can affect one eye or both eyes and is more common in the elderly, as muscles in the eyelids may begin to deteriorate. One can, however, be born with ptosis.
Acquired ptosis is most commonly caused by aponeurotic ptosis. This can occur as a result of senescence, dehiscence or disinsertion of the levator aponeurosis. Moreover, chronic inflammation or intraocular surgery can lead to the same effect. Also, wearing contact lenses for long periods of time is thought to have a certain impact on the development of this condition.
Aponeurotic and congenital ptosis may require surgical correction if severe enough to interfere with vision or if facial looks, cosmetics is a concern. Treatment depends on the type of ptosis and is usually performed by an ophthalmic plastic and reconstructive surgeon, specializing in diseases and problems of the eyelid.
Surgical procedures include:
Non-surgical modalities like the use of "crutch" glasses or special scleral contact lenses to support the eyelid may also be used.